Our research
Finished projects

Scientific project leader of external evaluation
Operative project leader
Project execution
Leading institution
- Prof. Dr. Michael Hallek, Klinik I für Innere Medizin, Uniklinik Köln
Consortium leadership
- PD Dr. Michael Kusch, Klinik I für Innere Medizin & LebensWert e.V., Uniklinik Köln
Consortium partners
- Prof. Dr. Alexander Gerlach, Lehrstuhl für Klinische Psychologie und Psychotherapie, Universität zu Köln
- Prof. Dr. Ullrich Graeven, Krebsgesellschaft Nordrhein-Westfalen e.V.
- Prof. Dr. Stephanie Stock, Institut für Gesundheitsökonomie und Klinische Epidemiologie, Uniklinik Köln
- Prof. Dr. Martin Hellmich, Institut für Medizinstatistik und Bioinformatik, Uniklinik Köln
- Prof. Dr. Peter Haas, Medizinische Informatik, Fachhochschule Dortmund
- Prof. Dr. Jürgen Wolf, Centrum für Integrierte Onkologie Köln Bonn
- Uwe Schwarzkamp, LebensWert e.V.
- PD Dr. Marcel Reiser, Praxisgemeinschaft Internistischer Onkologie und Hämatologie, Köln
- Dr. Christina Hecker, Qualitätszirkel Dermato-Onkologie Köln
- Ralf Rambach, Haus der Krebs-Selbsthilfe – Bundesverband e.V.
- AOK Rheinland/Hamburg
- BARMER
- Techniker Krankenkasse, Landesvertretung NRW
Duration
- 10/2017 – 09/2021
Funding institution
- Innovationsausschuss beim Gemeinsamen Bundesausschuss (G-BA)
Project description
Over 420,000 people in Germany contract cancer every year. Of these, about 20% to 30% suffer from comorbid mental disorders and about 50% from anxieties and depression at the time of diagnosis and during therapy.
Although an integrated and cross-sectoral psycho-oncological care is nationally and internationally regarded as a standard, it is still not implemented in Germany.
Only 9% of 6,000 interviewed cancer patients stated that they received in-patient psycho-oncological care and 3% that they went to a cancer counselling center.
The aim of the project isPO is to develop, implement, and evaluate a psycho-oncological care programme. Therefore, structures, processes and results of care provision are described and transparently and comprehensibly documented. Quality assurance measures are conducted as well.
The specific patient-oriented goal is to reduce recurrent acute psychological stress reactions such as anxieties and depression of cancer patients within the first year after initial diagnosis. In the isPO programme, psycho-oncological care is given starting from the time of the cancer diagnosis and is provided cross-sectorally over a period of 12 months. This is done by coordinated, individualized psycho-oncological support and patient information in the conurbation of Cologne and in three rural regions in North Rhine-Westphalia. The provision of psychosocial and/or psychotherapeutic care for a cancer patient depending on his or her need is guaranteed by physician-led care networks.
As a cooperation partner in the project isPO, the IMVR conducts the independent evaluation of the care programme examining its effectiveness and quality.
The scientific monitoring is carried out as a prospective, process and outcome evaluation. Document analyses, qualitative and quantitative interviews with patients, care providers and other potential users of the isPO programme as well as analyses of health insurance data are carried out.
Publications
- Jenniches, I., Lemmen, C., Cwik, J.C. et al. (2020). Evaluation of a complex integrated, cross-sectoral psycho-oncological care program (isPO): a mixed methods study protocol. BMJ Open 10:e034141. doi: 10.1136/bmjopen-2019-034141
Scientific and operational project leader
Duration
- since 04/2020
Project funding
- The study is funded by the IMVR
Project description
More information coming soon.
Publications
- Hower, K.I., Pfaff, H., Pförtner, T.-K. (2021). Is time a healer? Course of demands during the COVID-19 pandemic in long-term care: A repeated cross-sectional survey in Germany. Journal of Public Health, DOI:10.1093/pubmed/fdab144.
- Pförtner, T-K., Pfaff, H., Hower, K. (2021) Will the demands by the covid-19 pandemic increase the intent to quit the profession of long-term care managers? A repeated cross-sectional study in Germany. Journal of Public Health. DOI: 10.1093/pubmed/fdab081.
- Ergebnisbericht: Pflegerische Versorgung in Zeiten von Corona – Drohender Systemkollaps oder normaler Wahnsinn?
- Hower, K., Pfaff, H., Pförtner, T.-K. (2020). Pflege in Zeiten von Corona: Onlinebefragung von Leitungskräften zu Herausforderungen, Belastungen und Bewältigungsstrategien. Pflege – Die wissenschaftliche Zeitschrift für Pflegeberufe, 33(4) (2020). DOI: 10.1024/1012-5302/a000752
- Beitrag im Monitor Pflege: Mehr als der „normale Wahnsinn“?, Monitor Pflege, 6, 16-18. (https://www.monitor-pflege.de/kurzfassungen/kurzfassungen-2020/mehr-als-der-201enormale-wahnsinn201c)
- Vortrag im Landtag Rheinland Pfalz bei der Enquete-Kommission 17/2 „Vorsorge- und Bekämpfungsmaßnahmen gegen die Ausbreitung des Coronavirus in Rheinland-Pfalz und Konsequenzen für die Pandemiepolitik” (2020). Pflegerische Versorgung in Zeiten von Corona – Drohender Systemkollaps oder normaler Wahnsinn?
- Grafik des Monats November 2020, ausgezeichnet durch das BGF Institut
Results reports
Scientific management of the subproject
Project implementation (project part IMVR)
Consortium leadership
- Martin Dichter, Ph.D (IfP)
- Prof. Dr. Sascha Köpke (IfP)
Consortium partners
- Prof. Dr. Stephanie Stock (IGKE)
- Prof. Dr. Martin Hellmich (IMSB)
Cooperation partners
- Uniklinik Köln
- Universität Lübeck
Duration
- 03/2021 – 02/2024
Funding institution
- Bundesministerium für Bildung und Forschung
Project description
Every second hospitalised patient is older than 60 years. As a result, the number of cognitively impaired patients in hospital settings is increasing. Hospitalisation, the associated care and treatment are often experienced as negative stress by people with cognitive impairments (CI). These patients feel ignored, helpless or threatened. Hospital staff is conceptually insufficiently prepared for the care of people with CI. There is often a lack of expertise. Nurses themselves describe the care of people with CI in hospital as physically and mentally demanding and stressful.
Person-centred care is a promising care model to meet the needs of people with CI during hospital care. However, in order to successfully implement and establish person-centred care approaches in the hospital setting, so-called “change agents” are needed.
The project “ENROLE-Acute” pursues the following goals:
- Participatory development of a complex intervention based on expanded nursing roles and interdisciplinary team building to implement person-centred care for hospitalised patients with CI.
- Implementation and evaluation of person-centred care to reduce or prevent prolonged hospitalisation, challenging behaviour, delirium and pain in people with CI and reducing the burden on carers.
Person-centred care will be implemented and evaluated in a cluster randomised controlled trial.
The IMVR is responsible for the process evaluation of person-centred care, e.g. surveys of the interdisciplinary teams and patients with CI in the participating wards are planned. In addition, the patients will also be surveyed with a baseline survey, several follow-up questionnaires and individual interviews.
The aim of the project is to reduce or avoid prolonged hospital stays, challenging behaviour, delirium and pain for patients with CI as well as nursing staff’s stress.

Scientific and operational project leader
Duration
- seit 04/2020
Project funding
- The study is funded by the IMVR
Project description
Background: Although the conditions for digital working environments have improved, working from home is uncommon in German organizations. However, with the sudden spread of COVID-19, organizations are faced with social distancing measures in order to prevent the spreading of the virus. Therefore, the existing attendance culture needs to be discarded and replaced by an increase of working from home.
The question is, whether times like these provide the needed incentive to embrace the ongoing digital transformation at the workplace and have a lasting effect on the organizational culture.
Aim: The objective of this research project is to conduct a longitudinal study about working from home and attendance culture during COVID-19. The focus lies on the investigation of the relationships between working from home, attendance culture and burnout. In the long term we will also examine whether the newly established practice of working from home will lead to a change in the attendance culture in German organizations.
Methods: Data collection is conducted via an online survey on the social networks LinkedIn, Facebook, and Instagram. The research project targets employees who work from home during the COVID-19 pandemic. Participants who have given consent will be contacted again for a second survey.
Additionally, a qualitative interview study will be carried out with the target group from the public sector. The goal of the qualitative study is to provide information about the working from home experiences during COVID-19 with a focus on the topics of resources, demands and health.
Project leader
Project execution
Cooperation partner
- Prof. Dr. Hans-Jürgen Andreß (Institut für Soziologie und Sozialpsychologie, Universität zu Köln)
- Dr. Bart De Clercq (Department of Public Health, Ghent University)
- Prof. Dr. Matthias Richter (Institut für Medizinische Soziologie, Martin-Luther-Universität Halle-Wittenberg)
- Prof. Dr. Alexander Schmidt-Catran (Institut für Soziologie, Goethe-Universität Frankfurt am Main)
Duration
- 01/2018- 12/2020
Funding institution
- Deutsche Forschungsgemeinschaft (DFG); Projektnummer: 388147695
Project description
The German labor market in Germany shows a positive development as employment rates have increased and unemployment rates decreased. Nevertheless, science and social organizations are alarmingly pointing to growing rates of precarious employment since the 1980s. Employment relationships that are associated with uncertainties and risks are regarded as precarious. These include non-standard working time arrangements (e.g. marginal employment or temporary employment), occupations associated with job insecurity as well as occupations based on insufficient income at household and individual level. National and international studies indicate that precarious forms of employment pose a higher health risk. Against the background of increasing flexibility in the labor market and the continuation of precarious employment relationships, an in-depth discussion and analysis of the health situation of precarious employees is indispensable.
- What is the current relationship between subjective health and various forms of precarious employment in Germany and how has it developed over time?
- How does the causal interaction between subjective health and various forms of precarious employment present from a longitudinal perspective?
- What relevance do occupational and non-occupational factors have for explaining the relationship between subjective health and different forms of precarious employment?
- What is the relationship between presenteeism and different forms of precarious employment?
- How do different courses of precarious employment in the employment biography relate to subjective health?
Analyses are based on data from the German Socioeconomic Panel (SOEP 1984-2014) for the and data from the BIBB/BAuA Employment Survey (2011/12). Based on a theoretical explanatory model, a trend analysis will be carried out using descriptive and multivariate secondary data analyses. Causal interactions between precarious employment and subjective health are investigated on a dynamic cross-lagged panel design. The proportions of occupational and non-occupational factors explaining the relationship between precarious employment and health are determined by means of a mediator analysis within the framework of logistic regression models. In addition, the relationship between precarious employment and presentism is theoretically elaborated and empirically investigated. For the first time, the courses of precarious employment in the employment biography are identified by means of a sequence data analysis and examined for health inequalities.
Precarious employment is increasingly discussed at the international level as a new social determinant of health. . By elaborating a comprehensive model and identifying paths and mechanisms to explain the relationship between health and precarious employment, the project contributes to an expansion of knowledge. The clarification of the causal relationship is particularly relevant for possible interventions.
Publications
- Pförtner T-K, Schmidt-Catran A (2017) In-work poverty and self-rated health in a cohort of working Germans: A hybrid approach for decomposing within-person and between-person estimates of in-work poverty status. Am J Epidemiol. doi: 10.1093/aje/kww218)

Scientific project leader
Project execution
Consortium leader
- PD Dr. Clara Lehmann, Prof. Dr. Fätkenheuer, Klinische Infektiologie, Klinik I für Innere Medizin, Uniklinik Köln
Consortium partners
- Prof. Dr. Martin Hellmich, Institut für Medizinische Statistik, Informatik und Epidemiologie, Universität zu Köln
- Peter Ihle, PMV Forschungsgruppe, Universität zu Köln
Cooperation partners
- AOK Rheinland/Hamburg
- BARMER
- pronova BKK
- DAK-Gesundheit
- Dr. Gillor, MVZ Innere Medizin
- Drs. Stechel und Juretzko
- Dr. Scholten, Praxis Hohenstaufenring
- Drs. Isernhagen, Qurishi und Römer, Gemeinschaftspraxis Gotenring
- Prof. Dr. Holtmeier, Krankenhaus Porz am Rhein gGmbH
- Prof. Dr. Reuter, Klinikum Leverkusen gGmbH
- Prof. Dr. Oette, Krankenhaus der Augustinerinnen gGmbH
- Prof. Dr. Seifert, Institut für Medizinische Mikrobiologie, Immunologie und Hygiene, Uniklinik Köln
Duration
- 04/2019 – 03/2022
Funding institution
- Innovation Committee (Innovationsausschuss) of the Federal Joint Committee (G-BA)
Projektbeschreibung
Many infections necessitate the use of intravenous antibiotics, sometimes over the course of several weeks. In case of an outpatient parenteral antibiotic therapy (OPAT), these antibiotics are administered at home by the patient or a caregiver. This allows patients to remain in a familiar environment and avoids a hospital stay. Despite these advantages, OPAT is rarely used in German patient populations.
In this project, the execution and practicability of an OPAT will be evaluated systematically using the Cologne metropolitan region as a model. There are three main work packages in the project. As a part of the first work package, patients with an infection will receive OPAT followed by an evaluation of the OPAT effectiveness. The data that is gathered will provide information about the success of OPAT and about the satisfaction of patients and treating physicians. The second work package includes a survey of established physicians in Cologne. In the third work package, the current care situation and the relevance of OPAT will be examined using an analysis of Statutory Health Insurance (SHI) data. For this secondary data analysis, the CoRe-Net database will be used.
The Institute of Medical Sociology, Health Services Research, and Rehabilitation Science (IMVR) are involved in the evaluation of OPAT and will conduct the survey with established physicians. As a part of the evaluation, the satisfaction of patients will be conducted with a quantitative survey. To gather more in-depth information, we will also conduct interviews with selected patients based on the survey data. Furthermore, the IMVR will conduct two focus groups to identify the reasons why an implementation was successful to better inform the clinical providers. Based on the results of the focus groups, a quantitative questionnaire will be developed to identify the current attitude of established physicians in Cologne and possible barriers of OPAT implementation.
If successful, the project should help to identify the potential of the OPAT for Germany. If positive effects and feasibility can be demonstrated in the Cologne metropolitan area, the OPAT could become an important treatment option that is beneficial for many patients. The findings from this study, as well as developed concepts and structures, can later be transferred nationwide.

Project management
Project employees
Duration
- 06/2020 – 11/2021
Funding
- Federal Ministry of Education and Research (BMBF)
Project description
With regard to the Corona pandemic, the hospital is the main focus of attention. Approximately 5-15 percent of people who are tested positive for SARS-CoV-2 have a course of disease that requires hospital consultation or admission to hospital. If possible, minor cases of COVID-19 infection should be treated exclusively on an outpatient basis. The outpatient sector thus takes over the main quantitative burden of care for COVID-19 patients on the one hand and serves as the first point of contact for those affected, especially in the general practitioner sector, on the other hand. In addition, the cancellation of elective procedures in hospitals leads to a shift of inpatient cases to outpatient care, where they are (further) treated in the sense of conservative therapy. Under certain circumstances, this can lead to a deterioration in the patients’ state of health, as well as to a change in the use of visits to practices as a result of public risk communication.
COVID-GAMS is a health care research study that examines the impact of the COVID-19 pandemic on the outpatient sector. It investigates organisational, economic and interpersonal challenges as well as the direct effects on patient care from the perspective of general practitioners.
The following questions are to be answered in an online survey:
1. Which organisational challenges are experienced in adapting to the crisis?
2. Which economic challenges for the practice show up concretely?
3. Which effects does the crisis have on patient care?
4. Which interpersonal challenges does the crisis bring with it?
Since the challenges of the COVID-19 pandemic may differ in detail between the individual disciplines within the outpatient sector, general practitioners of different specialties will be interviewed. There will be three survey waves. In each of which 18,000 medical specialists will be contacted:
|
General practitioners |
6.500 |
|
Medical specialists for internal medicine: |
|
|
Cardiologists |
1.000 |
|
Gastroenterologists |
500 |
|
Specialists in Paediatricians |
2.000 |
|
Specialists in Gynaecologists |
2.000 |
|
Specialists in ENT |
2.000 |
|
Dentists |
4.000 |
The survey waves are carried out in the sense of a trend analysis at three survey dates (2 months, 5 months and 13 months after the start of the study).
The results should contribute a better preparation of the outpatient sector for epidemics and pandemics in the future. At the same time, they can help to react early to possible problems that are already apparent in the outpatient sector. In particular, potential deteriorations in the health situation of patients due to a currently suboptimal care situation as a result of the COVID 19 pandemic should be mentioned here. At the same time, opportunities for a long-term improvement in care are identified, e.g. as a result of digitalisation and the increase in telemedical forms of treatment.
Contact and further informations

Scientific project leader
Operative project leader
- Anna Choi
Project execution
- Lara Lindert
- Lara Schlomann
Co-operation partners
- BKK Federal Association
- 15 company health insurances and 22 companies
- Institute of Medical Statistics and Computational Biology (IMSIE)
- Insurance Agencies of the German Statutory Pension Insurance
- German Society for Medical Rehabilitation (DEGEMED)
Duration
- 04/2017 – 03/2021
Funding institution
- Innovation Committee (Innovationsausschuss) of the Federal Joint Committee (G-BA)
Project description
BGM-innovativ for employees with musculoskeletal disorders is a response to the specific needs for healthcare in companies. The objective of the program is to offer sick or vulnerable employees targeted support tailored to their individual needs during recovery and the provision of healthcare. This will be ensured by cross-carrier and cross-sector coordinated healthcare.
The various social security carriers are faced with similar needs for action in preventive, curative and rehabilitative treatment, care and support. However, their measures have been taking place in a largely disjointed and uncoordinated manner so far. For this reason, BGM-innovativ intends to establish close cooperation and coordination between the relevant health insurance carriers, pension providers and companies. Thus BGM-innovativ is an approach to combat insufficient cross-sector healthcare cooperation for employees with musculoskeletal disorders.
The program aims to avoid disease and chronification, reduce disease duration and days of absence and to permanently maintain capacity for work. Companies and employees will be supported in the field of corporate healthcare management (BGM) by healthcare management oriented to each individual workplace situation. A central innovation of BGM-innovativ is the case manager of the company health insurance funds, who is the personal contact for policy holders, organizes specific and appropriate healthcare and coordinates the interfaces between the various parties. The case manager leads the employees through the healthcare process and involves them in all planning and decision-making processes. BGM-innovativ has a multimodal structure and intends to establish workplace-relevant, individualized and cross-sector healthcare measures. Depending on the stage of the disease and the impact on the employee, these measures may be early intervention, rehabilitation or reintegration.
We refer to BGM-innovativ as a metaconcept; instead of creating additional structures and services, it strengthens cross-system thinking and the awareness of the various parties. Key factors like the case manager, who takes over a guiding role for policy holders in the healthcare process, will be implemented once and can then be applied in further contexts, indications, sectors, regions and health insurance funds. Whereas the supported project primarily focusses on musculoskeletal diseases, should the project be successful, the concept could be applied to the healthcare processes of different, high-prevalence diseases.
IMVR will coordinate the evaluation of the BGM-innovativ program. The design of the study employs a mixed-method approach and consists of both an accompanying, process-oriented (formative) and a result-oriented (summative) evaluation.
Summative evaluation using a randomized trial
The summative evaluation aims to check the effectiveness of the program using a randomized controlled trial (RCT). The participants are randomly divided into two treatment groups before the program commences for this purpose. All participants receive a standardized questionnaire at the beginning and in the end of the program. Furthermore, additional key figures, like information regarding incapacity for work, are evaluated. Using the pre-post comparison and the comparison of the two groups in each module, robust conclusions can be drawn on the effectiveness of the program. Additional qualitative interviews with some participants supplement the summative evaluation.
Formative evaluation using qualitative methods
Formative evaluation with qualitative implementation research meant to identify those factors conducive and restrictive to implementation of the program will take place alongside it. Relevant parties (like case managers and company physicians) will be asked about their subjective experiences of implementation of the program in focus groups and expert interviews. These surveys will take place at several points throughout the project to obtain as comprehensive a picture as possible.
The results of the evaluation will make an important contribution to evidence-based corporate health and healthcare management. They will promote cross-carrier and cross-sector cooperation between the various healthcare parties and therefore improve the targeted and individual support of sick employees during recovery and in the provision of healthcare.
Scientific project leader
- Prof. Dr. Holger Pfaff
- Ute Karbach
Operative project leader
Duration
- 06/2018 – 04/2021
Project funding
- Die Studie wird aus Eigenmitteln des IMVR finanziert.
Project description
Background: The influence of social factors, such as subjectively perceived participation, loneliness, and social support on (multi-)morbidity, has been little studied. It seems particularly striking that increasingly these factors are being identified as contributors to morbidity and mortality and are, therefore, growing into a problem of epidemiological magnitude. In a meta-analysis based on 70 international quantitative studies, Holt-Lundstad et al. (2015) identified an average 28% to 32% higher mortality risk, depending on the social factors of subjective loneliness and objective isolation. Such an analysis with explicit reference to (multi-)morbidity has so far been lacking.
Aim: The project aims to develop theory-based effect models of social factors such as subjective loneliness and social support on morbidity and to test them empirically. The psychosocial mechanisms postulated by Berkman (2000) and Holt-Lunstad’s (2018) socio-ecological model are considered the basis of the effect models. The impact models are extended by the particular focus on multimorbidity and ageing. Two different data sources are used for the empirical review. The distinction and choice of secondary data are thereby based on the different life situations to consider regarding multimorbidity.
- The GSPE-III is used to test the effect models in the context of persons in the last third of earning capacity. For this purpose, there is a cooperation with Prof. Dr. Matthias Bethge
- For the studies based on older persons (age approx. > 65 years), the data sources of the German Center of Gerontology (DZA) are used.
Both data sets allow a longitudinal view of at least three survey waves so that the answer to causal questions is attempted.
-
Can social support positively influence the association between multimorbidity and mental well-being?
- Do prolonged episodes of loneliness favour the development of multimorbidity?
Furthermore, guided by the theoretical model, consideration will be given to other relevant (confounding) characteristics. Thereby, methodological issues of empirical testing will be brought to the fore.
Outlook: In addition to answering the analysis questions, the results will guide future projects in the context of morbidity and social factors in their evaluation design. For this purpose, the results will be compared with the innovation fund project MamBo.
Scientific project leader
Operative project leader
Project execution
- Simone Richter
Co-operation partners
- Pronova BKK
- Regionales Gesundheitsnetz Leverkusen (RGL)
- Organisationsberatung (N.N.)
- Institut für angewandte Gesundheitsforschung Berlin GmbH (InGef)
Duration
- 07/2017 – 04/2021
Funding institution
- Innovation Committee (Innovationsausschuss) of the Federal Joint Committee (G-BA)
Project description
Adequately and efficiently treating patients with complex multimorbid disease situations requires well-structured, informed and cross-indication treatment. Disease-specific healthcare structures cannot be provided for every disease. For this reason, a disease-spanning metastrategy will be pursued and the necessary structures established in the MamBo Project.
Public health and individual goals will be focused on in equal measure for this cross-indication collective healthcare. Framework conditions will be created to enable patient-relevant and comprehensive sector information to reach the physician administering treatment. The cross-practice delegation of near-patient and coordinative tasks thus relieves the burden on the physician.
The structure required for this innovation in healthcare is composed of demand management on the part of the payer, of care management on the part of the physician network involved and of continuous improvement processes, which are discussed in regular meetings with those involved in the process.
The aim of the project is, firstly, to identify those factors conducive and restrictive to the implementation of this innovation in healthcare in an accompanying formative evaluation. Secondly, structure, process and result quality will be examined from multiple perspectives in a summative evaluation. This examines whether a change in healthcare quality and healthcare efficiency is effected by the MamBo structure in the Leverkusen region (Germany) and how cooperation in the various disciplines is developing.
Within the framework of the formative evaluation, annual focus groups and individual interviews with those involved in the process will be conducted, recorded, transcribed, assessed with regard to content analysis and then presented in results workshops.
Various primary and secondary data sources will be used in the summative evaluation. Postal surveys of patients, physicians and practice employees conducted at two points in time will enable a pre-post comparison. Health insuerers’ administrative data (claims data) of the MamBo population will be compared with those of a comparative population in various capacities in a semi-experimental design. The comparative population will be formed according to the propensity score matching method. In addition, secondary data from documents of the physician network will be analyzed in the summative evaluation.
Scientific project leader
Operative project leader
Project execution
- Isabell Schellartz
Scientific cooperation partner
- Dr. Gero von Gersdorff, Dr. Katherine Rascher (Department II of Internal Medicine – QiN group, University Hospital of Cologne)
- Prof. Dr. Martin Hellmich, Christina Samel (Institute of Medical Statistics and Computational Biology, University of Cologne (UoC))
- Prof. Dr. Thomas Mettang (Center for Kidney Disease and Hypertension, Wiesbaden)
- Prof. Dr. Stephanie Stock, Dusan Simic, Kristina Lorrek (Institute for Health Economics and Clinical Epidemiology, Cologne University Hospital, UoC)
- Krankenkasse DAK Gesundheit
- Siemens Betriebskrankenkasse (SBK)
Duration
- 05/2017 – 04/2020
Funding institution
- Innovationsausschuss beim Gemeinsamen Bundesausschuss (G-BA)
Project description
From a medical perspective, peritoneal dialysis (PD) and hemodialysis (HD) are equivalent treatment options for patients with chronic kidney disease (CKD). Findings show that PD rates vary considerably worldwide (e.g., Hong Kong 79.4%, Sweden 23.8%, Germany 5.4%, and Luxembourg 0.7%). The objective of the project is to identify causal factors for the low PD rate in Germany. The effect of these factors can be the promotion or inhibition of PD from different perspectives of patients, physicians, nurses, and sickness funds. In this cross sectional study, our focus is on the health care situation of dialysis patients at a local level as well as the different costs and cost categories (HD vs. PD). Furthermore, we analyze the identification and weights of factors of patients, physicians, and nurses that are relevant for modality choice. The study is funded by the Innovation Committee of the Federal Joint Committee.
The health care situation is represented by secondary data analysis. Data resources consist of panel medical care accounting data produced by the Central Research Institute of Ambulatory Health Care of the National Association of Statutory Health Insurance Physicians; claims data from two cooperating statutory health insurance companies; and quality assurance data from KfH (QiN – Quality in Nephrology), an ambulatory dialysis provider in Germany. Using a mixed methods design, we conduct qualitative individual interviews with patients and focus groups with nephrologists and nurses as well as a quantitative survey using a standardized questionnaire. Different questionnaires are targeted at health care professionals (physicians, dialysis nursing managers, and dialysis nursing staff) and patients. This data enables the identification of causal factors for the uptake of PD as well as its distribution and relevance.
We expect a representative quantitative analysis of factors influencing the treatment choice for or against PD. Finally, an action plan including practical solutions is derived from the results of this analysis. These results can reveal approaches at different levels of health care delivery, including at the organizational level with internal and external organizational structures and processes and at the individual level of physicians and patients. In addition, the results open up a major discussion for all players in the health care sector (e.g., dialysis providers, funders, etc.).
Scientific project leader
Operative project leader
Project execution
- Kerstin Dittmer (deputy operative project leader)
- Dr. Kira Hower
Scientific collaboration partners
- Prof. Dr. Martin Hellmich, Christina Samel (Institut für MProf. Dr. Martin Hellmich, Christina Samel (Institute of Medical Statistics and Computational Biology, University of Cologne)
- Hilde Schulte (Frauenselbsthilfe nach Krebs Bundesverband e.V.)
- Prof. Dr. Rita Schmutzler (Center for Hereditary Breast and Ovarian Cancer, University Hospital Cologne
Duration
- 05/2017 – 04/2020
Funding institution
- Innovation Committee (Innovationsausschuss) of the Federal Joint Committee (G-BA)
Project description
The discharge of patients from breast cancer centers has to be prepared adequately to guarantee a successful transition to general practitioners. However, the discharge process is often affected by unnecessary waiting times. Patients evaluate the process rather negatively. In addition, the process is challenging for the involved personnel.
Value Stream Mapping aims to improve the discharge process. The methods visualizes complex work flows and thereby intents to create a more efficient and value-adding process. For the patient, value-adding could imply, for instance, a follow-up treatment within the breast cancer center.
Research question: The project at hand considers the question whether the discharge process in breast cancer centers can be improved by using Value Stream Mapping. The project aims to evaluate the method of Value Stream Mapping when applied to the discharge process of breast cancer centers.
Four certified breast cancer centers in North Rhine-Westphalia form project teams out of employed representatives of all involved occupational groups (e.g. administration, nursing, medical staff). The discharge is visualized together with a trained facilitator. The project team analyzes the current state value stream map together with a patient representative. The time needed for the discharge is determined, process steps are analyzed and causes of missing value for the patient are identified. Based on this information, the project team improves the discharge process and creates a renewed future state value stream map. Finally, the new process will be implemented.
The intervention is evaluated based on a before-after-follow-up study design. The discharge process is measured in the four participating breast cancer centers before the intervention, directly afterwards and six months later. The evaluation is carried out through time measurement and questionnaires for patients and employees. These data are analyzed by descriptive and inferential statistical methods.
Project direction and execution
Duration
- 02/2014 – 2020
Project funding
- The study is funded with IMVR’s own resources
Project description
At the time of the first breast cancer diagnosis, the majority of affected women and men are still at an employable age (median: 60 years). Work is associated with higher quality of life, more self-esteem and a sense of normality. Therefore, returning back to work must be a declared aim for all patients who are employed prior to diagnosis. Studies have shown that oncologic patients often have problems in the work context. The probability of returning back to work is related to many different factors, for example age at the time of diagnosis, the severity of the disease and the type of treatment. So far, not much is known about the variation between hospitals in respect to the percentage of patients returning back to work and the length of sick leave. The aim of the project is to analyze possible variations between hospitals and assess the extent to which such differences can be explained by the characteristics of particular hospitals. This project is based on cooperation between the IMVR and the AOK Rheinland/Hamburg.
Given patients’ agreement to link their health insurance data with the data from the patient survey at the breast centers (“Routine survey”) these data basis are being linked und analyzed with reference to occupational rehabilitation after two and after five years.
Scientific project leader:
- Dr. Lena Ansmann
Operative project leader
- Dr. Kira Hower
Scientific collaboration partners
- Prof. Dr. Stephanie Stock, Vera Vennedey (Institut für Gesundheitsökonomie und Klinische Epidemiologie)
- Prof. Dr. Ludwig Kuntz, Hendrik Hillen (Seminar für ABWL und Management im Gesundheitswesen)
Duration
- 02/2017 – 01/2020
Funding institution
- Federal Ministry of Education and Research
Project description
Health care systems are under pressure to organize care around patients’ needs with strained resources. Several studies reveal that care is primarily supply-driven rather than patient-centered. Therefore, value-based health and social care aims to redesign care delivery around patient-centeredness whilst taken the resources spent into consideration.
OrgValue is one of three scientific projects of the Cologne Care Research and Development Network (CoRe-Net).
The organizations in Cologne caring for vulnerable patient groups studied in the subprojects LYOL-C and MenDis-CHD are examined in OrgValue using a mixed methods approach.
The implementation status of patient-centeredness and resource orientation as well as its facilitators and barriers are assessed through face-to-face interviews with decision makers from HSCOs in Cologne. Additionally, patients’ understanding of patient-centeredness and their preferences and needs are surveyed conducting focus groups and face-to-face interviews. This opens up a comparison of organizations’ and patients’ pPublications about the resultsdness.
The qualitative results provide the basis for a quantitative survey with decision makers from all HSCOs in Cologne. All examinations include questions on patient-centeredness, resource orientation and determinants of implementation like organizational climate and culture. The development of a diagnostic and feedback-tool for self-evaluation out of the aforementioned survey is taken into consideration.
Scientific project leader
Project execution
Consortium leadership
- Prof. Dr. Roman Rolke, Direktor Klinik für Palliativmedizin, Uniklinik RWTH Aachen
Consortium partner
- Univ.-Prof. Dr. med. Raymond Voltz und Dr. Dr. Julia Strupp, Klinik für Palliativmedizin, Uniklinik Köln
- Univ.-Prof. Dr. med. Lukas Radbruch, Klinik für Palliativmedizin, Uniklinik Bonn
- Univ.-Prof. Dr. Holger Pfaff und Dr. Nadine Scholten, Institut für Medizinsoziologie, Versorgungsforschung und Rehabilitationswissenschaft (IMVR) der Universität zu Köln
- Prof. Dr. Martin Hellmich, Leiter der Abteilung Medizinische Statistik und Epidemiologie, Institut für Medizinische Statistik, Informatik und Epidemiologie, Universität zu Köln
- Prof. Dr. Christian Rietz, Professur für Forschungsmethodik, Leiter des Department Heilpädagogik und Rehabilitation, Universität zu Köln
- Dr. rer. soc. Ingrid Schubert, PMV Forschungsgruppe, Kinder- und Jugendpsychiatrie, Universität Köln
Cooperation partner
- AOK Rheinland/Hamburg
Duration
- 06/2017 – 05/2019
Funding institution
- Innovation Committee (Innovationsausschuss) of the Federal Joint Committee (G-BA)
Project description
German outpatient palliative care is divided into general outpatient palliative care (AAPV) and specialized outpatient palliative care (SAPV). Both forms enable ill and dying persons to spend their remaining time at home so that they can die in a familiar environment. The aim of outpatient palliative care is to provide an increase in quality of life and support patients and their relatives to preserve their self-determination. Additional goals are the alleviation of symptoms such as the reduction of pain. SAPV is based on high standards in providing care and requires an interdisciplinary approach. Therefore, physicians exclusively prescribe SAPV to patients with a complex symptomatology.
The chairs of palliative medicine of Aachen, Bonn, and Cologne aim to evaluate SAPV in the Province of North Rhine. The project contrasts SAPV with AAPV. There are three main research goals. The first part deals with the analysis of administrative health insurance data. So it is focused on patient characteristics and health care tracks as well as health care differences between patients that receive AAPV or SAPV. The second section examines SAPV and AAPV from the patient’s point of view as well as from the perspective of their relatives and palliative care providers.
The third part of the project is located in the Institute of Medical Sociology, Health Services Research, and Rehabilitation Science (IMVR). The institute investigates distinctive features of SAPV and AAPV according to the opinion of general practitioner and oncologists in the outpatient sector. The objective is to analyze decisions of both disciplines for prescribing SAPV instead of AAPV and to define the term “complex symptomatology.” The design of the study is based on mixed methods. The initial stage of the project process includes qualitative expert interviews and focus groups. Afterwards, a quantitative questionnaire will be developed on the basis of the qualitative research results.
Scientific project leader
Project execution
- Sara Söling
Consortium leadership
- BARMER
- Overall project management: Petra Kellermann-Mühlhoff
Cooperation partner
- KV Westfalen Lippe
- Prof. Ferdinand Gerlach, Institut für Allgemeinmedizin, Universität Frankfurt
- Prof. Hans Trampisch, Abteilung für Medizinische Informatik, Biometrie und Epidemiologie, Medizinische Fakultät der Ruhr-Universität Bochum
- Prof. Wolfgang Greiner, Lehrstuhl für Gesundheitsökonomie und Gesundheitsmanagement, Universität Bielefeld
- Dr. Ingrid Schubert, PMV forschungsgruppe, Universität Köln
Duration
- 10/2016 – 09/2019
Funding institution
- Innovationsausschuss beim Gemeinsamen Bundesausschuss (G-BA)
Project description
Many elderly people suffer from multimorbidity and require several drugs simultaneously. The medical treatment of these patients brings with it an increased risk of drug interaction, side effects and medication errors.
AdAM contains specially developed software, which offers physicians digital support to improve the quality, safety and coordination of pharmacotherapy and healthcare management. The software has various functions, such as:
- Extracting treatment-relevant patient information from health insurance carrier routine data in real time with the patient’s informed consent
- Conducting electronically supported drug safety tests and printing the required standard German drug charts in various languages for patients
- Sending automatic risk warnings in the event of medication errors
- Automatic notifications when outpatients are admitted for inpatient treatment and coordinating drug administration with the hospital
The IMVR will conduct the formative evaluation of the new AdAM form of healthcare, thus presenting which factors conducive and restrictive to implementation may be observed in the application of this digitally supported pharmacotherapy management. Participating general practitioners in the control group and intervention group will be asked questions regarding those factors conducive and restrictive to implementation (user-friendliness of the software, obstacles) in guided telephone interviews and focus groups will be organized with those who have been using the application for a while and those who have started using it recently. Based on the results of this qualitative data collection, a postal survey (quantitative) will be developed and employed in participating practices to record factors relevant to physicians and practices. Qualitative evaluation will either be content analytical or qualitative descriptive, depending on the issue being addressed. The survey will be descriptive.
Project leader
Projekt staff
- Dr. Anika Nitsche
- Dr. Timo-Kolja Pförtner
- Dr. Silja Fiedler
Co-operation partner
- Institute of Health Promotion and Clinical Movement Science (German Sport University Cologne, DSHS), Prof. Dr. Ingo Froböse
- Institute for Health Economics and Clinical Epidemiology (IGKE), Prof. Dr. Stephanie Stock)
Sponsors
- Federal Ministry of Education and Research (BMBF); Support code: 01EL1425B
- Trisearch – BMBF Research association of Primary prevention and health:
Duration
- 02/2015 – 01/2018
Funding institution
- Federal Ministry of Education and Research (BMBF
Project description
When it comes to health promotion in companies, managers play a key role. Managers can not only influence the working environment of their employees, they can also act as role models through their own health behavior. Many studies confirm the link between managerial behavior and employee health.
Furthermore, it should not be neglected that managers themselves also represent an important target group for health-promoting measures. Studies found that managers are more frequently exposed to particularly high levels of stress und interruptions, as well as to large workload with time constraints than other employees.
Consequently, the development of manager health literacy can be seen as a vital component for the promotion and protection of both their own employability and the employability of their employees.
Aim of the project is the conception, implementation and evaluation of an evidence-based training program for promoting health literacy of managers.
Therefore the following questions arise:
- How can a basic qualification in health literacy for managers with an acceptable, feasible and promising training program be achieved?
- How effective is the training program for managers?
- Does a basic qualification in health literacy affect the (physical and mental) health of managers?
For the evaluation, pre- and post-surveys in a randomised controlled intervention trial are planned.
With its substantive and methodological evidence-based approach, the proposed project offers the possibility of further research.
Results
Below you will find topic-specific results from the HeLEvi research project.
Factsheet I : Promoting health literacy among managers – an evidence-based training program (german).
Factsheet II: Factors for the promotion of health literacy (german)
Factsheet III: Results of a randomized controlled trial (german)
- Fiedler, S., Pförtner, T.-K., Nitzsche, A., McKee, L. & Pfaff, H. (2017). Health literacy of commercial industry managers. An exploratory qualitative study in Germany. Health Promot Int1, 1–11.
- Fiedler, S., Pfaff, H., Soellner, R. & Pförtner, T.-K. (2018). Exploring the association between health literacy and psychological well-being among industry managers in Germany. J Occup Environ Med, 60 (8), 743–753.
- Fiedler, S., Pfaff, H., Petrowski, K. & Pförtner, T.-K. (2019). Effects of a Classroom Training Program for Promoting Health Literacy Among IT Managers in the Workplace: A Randomized Controlled Trial. J Occup Environ Med, 61 (1), 51–60.
Scientific project leader
- Dr. Ingrid Schubert (PMV-Forschungsgruppe)
- Prof. Dr. Holger Pfaff
Operational project management (IMVR)
Project execution (IMVR)
- Melanie Zirves
Cooperative partner
- Prof. Dr. Wilhelm Niebling, University of Freiburg
- AOK Baden-Württemberg
Duration
- 09/2017 – 07/2018
Funding institution
- Ministerium für Arbeit und Sozialordnung, Familie, Frauen und Senioren Baden-Württemberg
Project description
The study focuses on the rehabilitative health care for geriatric patients in the Federal State Baden- Württemberg (Germany). The aim of the research project is to generate evidence of the realization of the potentials of rehabilitative health care for geriatric patients. For this, it is a necessary prerequisite to identifying potentials of rehabilitative health care for geriatric patients in order to offer appropriate rehabilitative treatments for those patients.
Our findings will contribute to the further development of rehabilitative health care for geriatric patients (in Baden-Württemberg).
Scientific project leader
- Dr. Lena Ansmann
- Prof. Dr. Holger Pfaff
Operative project leader
- Kira Hower
Cooperation partner
- Information and aid in drug issues e. V. Wesel, Jörg Kons and Sandra Groß
Funding institution
- Auridis GmbH
Duration
- 07/2017 – 12/2018
Project description
Currently, about 50,000 children of drug-addicted parents are living in Germany. Repeatedly, the media reports tragic deaths and cases of neglect of infants and young children of drug addicts. To consider the situation of children of addicts, an opening and widening of the activities of drug-counseling centers is necessary. So far, only 10% of drug-counseling centers in Germany offer activities directed to children of drug-addicted parents or involve them in drug and addiction support. Accordingly, drug counseling is not prepared to care for children of addicts.
Implementing this topic into the existing structures and processes of drug and addiction support is a complex task. The Fitkids Program was developed by a drugs counseling center in Wesel with this in mind. Fitkids offers a supportive framework to continuously maintain dialog on the topic in drug counseling centers and to enable training, information and implementation processes.
The ultimate objective of Fitkids is to enable children with drug-dependent parents to grow up healthily and in an age-appropriate way. The program aims to achieve this by sustainably implementing children-oriented structures and processes in drug-counseling centers (read more).
Following the results of a formative evaluation of the Fitkids Program, the implementation process was optimized, and the Institute of Medical Sociology, Health Services Research and Rehabilitation Science (IMVR) of the University of Cologne was commissioned with a further evaluation (2015 – 2017). This “Evaluation study of the Fitkids program for children orientation in drug counseling centers” (EvaFit) was conducted as a summative evaluation to investigate the implementation of the program in 15 drug counseling centers and 10 drug counseling centers, which piloted the program 4-5 years ago, from the perspective of management and employees.
Cross-sectional qualitative study with semi-structured individual interviews with parents and children
As the Fitkids Program is a complex intervention, further evaluation studies are needed (EvaFit II) to comprehensively evaluate the program. In this second stage of evaluation, the quality of program provided and its effects will be evaluated from the perspective of the target group concerned – parents suffering from drug addiction and their children.
The evaluation has the primary characteristics of a summative evaluation; i.e. a comparison between postulated and achieved goal attainment within the Fitkids Program.
The assessment tools used in the study will be developed based on the results of EvaFit, previous experience of the evaluating researchers and the current state of research. 30 semi-structured individual interviews with parents addicted to drugs or their children are planned.
Scientific leader
Operative leader
Duration
- 10/2018 – 11/2019
Project funding
- Central Institute for Statutory Health Insurance in Germany (Zi)
Project description
Due to its cross-sectoral character, the affiliated physician system is a long-standing care model that can contribute to solving the interface problems in the German healthcare system. The affiliated physician is a contract physician who works at the hospital but is not employed. He uses the infrastructure of the hospital to treat his patients as full or partial inpatients. In this way, he can provide his outpatients with one-stop care in the event of surgical requirements. The flexibility created by the cross-sector character of the affiliated physician system makes it particularly suitable for use in structurally weak areas. This form of care is therefore currently and in the future of great relevance and potential for ensuring inpatient care.
Despite the advantages of this care model, there are few incentives, especially on the part of inpatient providers, to maintain departments staffed by affiliated physicians. This is particularly evident in the decreasing number of inpatient departments as well as inpatient physicians. The project investigates the role of inpatient departments in German acute care hospitals.
In addition to describing the differences in performance between affiliated, main and mixed departments, the opening and closing of affiliated departments will be described and their determinants identified. On a regional level, the importance of inpatient departments for inpatient care will be highlighted. Thus, the project examines the role of general practitioners from the perspective of organizational theory (meso) as well as the social relevance of this form of care through regional analyses (macro).
Project leader
Project execution
- Dr. Antje Dresen
- Dr. Susan Lee (operational project management)
- Markus Alich (administrative project management)
- Natalia Cecon (PhD student)
Duration
- 02/2018 – 01/2019
Project description
Background: Due to higher survival rates and the further development of therapeutic options in oncology, breast cancer patients can return to their old lives earlier. Today, however, oncological diseases are largely presented as chronic diseases, and patient reported outcomes (PRO) are therefore given a central position in patient surveys. The measurement of PRO is important during and after treatment to assess patients’ experiences and opinions in this context. The importance of PRO and quality of life after cancer underscore the relevance of this project.
Research Aim: The aim of the project is to gain knowledge about PRO in breast cancer patients 12 months after breast surgery. Patients who took part in the patient survey of the NRW Breast Centers are interviewed again 12 months after the operation by the Institute for Medical Sociology, Care Research and Rehabilitation Science (IMVR). This quantitative, postal survey is intended to assess the patients’ state of health, information needs and PRO. Based on the collected data, information can be derived regarding the physical and psychological quality of life and about the subjective state of health 12 months after the operation. Furthermore, the research group hopes to use the study design to generate comparative data between the first (post-stationary) and second waves of the survey (12 months after the operation) in order to be able to analyze changes over time.
Method: Informed consent to participate in the follow-up survey was collected together with the consent to the annual patient survey in the NRW breast centers. If the patient agreed to participate in the follow-up study, a standardized questionnaire with an addressed and stamped envelope was sent to the patients 12 months after the operation, with the request to complete the questionnaire within the next two weeks and send it back to the IMVR. In order to be able to link the follow-up data with the first patient survey data, the patients received an identification number, which is provided on the questionnaire. As with the routine patient survey in the NRW breast centers, the survey is based on Dillman’s Total Design Method. The data is then documented, tested for quality assurance, and evaluated at IMVR.
Outcomes: The directors of the operational sites of the breast centers will receive the results of the data in the form of a report. The results can be used from the clinical perspective of breast centers to monitor treatment success and symptoms over time in order to improve the quality of care for breast cancer patients who have undergone surgery in a NRW breast center.
Scientific and operational project management
- Dr. Antje Dresen
- Dr. Susan Lee
- Dr. Eckhard Korsch (Holweide Children’s Hospital, Cologne)
Duration
- 09/2017 – 06/2019
Project Description
In the German federal state of North Rhine-Westphalia, one in eight rescuers has been a victim of violence, and more than one in two has reported experiencing abuse or insults while in service. The probability of such incidents increases in the evening and night hours and under the influence of alcohol and drugs, making the work of emergency doctors, police officers, firefighters, disaster control and rescue services more difficult (dpa/may/aertzeblatt.de). The German government has recently decided to impose harsher penalties for attacks on this group of people. However, general practitioners and hospital doctors are not included under the protection of this law.
There have also been indications of acts of aggressions and violence experienced within this group, although this topic is rarely acknowledged in public discourse. However, the daily experiences of doctors in clinics testify to situations of highly emotional and sometimes aggressive communication. In the pediatric clinics in particular, “difficult interactions” with parents or relatives of children to be treated have been reported. This subject area, however, has rarely been researched. Only two studies by Mackin et al. (2001) and Korsch et al. (2003) have dealt with aggressive behavior of parents and relatives towards hospital doctors in pediatrics. More than half of the pediatricians of one study, conducted by Korsch et al (2003), reported situations – median once a year – in which doctors saw themselves as the target of an aggressive action by parents or relatives. Against this background, another survey of pediatric hospital physicians was conducted to reveal the facets and consequences of aggression and violence in this setting, as well as over time.
Have the addressed doctors ever experienced an aggressive action by parents or relatives, and if so, when and in what form? In addition, this study explored whether acts of aggression resulted in a personal burden or whether they influenced the pediatric work of the physicians, as well as how the affected persons behaved after such a case.
At the end of 2017, questionnaires were sent to the assistant spokespersons of all pediatric departments and pediatric clinics in Germany. The questionnaires asked whether pediatricians experienced forms of aggressive action such as exerting pressure, insulting, threatening physical violence, attempts to use violence or violent acts. The respondents were also able to specify the nature and content of the insult, type of threat, etc. through open-ended questions.
A first impression of the data shows that experience with aggressive situations in the pediatric field has increased compared to studies cited in previous years. This study further explores the frequency and nature of the aggressive incidents and the medical behavior of the physicians. This ranges from calming or de-escalating a given situation to substantive clarification. Further topics that are discussed include aggressive counter-reactions, the involvement of colleagues or the police, the ignoring of family members, and ultimately leaving the place of work. The findings of this study demonstrate the relevance of the problems of aggression and violence in the context of pediatric work.
Publication: Dresen A., Lee S., Pfaff H., Weiß M., Korsch E. (2020): “Crazy bitch“ – Erlebte Aggression und Gewalt im Klinikalltag von Kinderärzten. Monatsschrift Kinderheilkunde 2020, https://doi.org/10.1007/s00112-020-01034-3.
Scientific direction
Project execution
Duration
- 01/2017 – 03/2018
Project funding
- Central Research Institute of Ambulatory Health Care in Germany (Zi)
Project decription
The German health-care system has traditionally been segregated into an inpatient and outpatient care sector. Due to negative effects of this segregation, especially the integration of care in sparsely populated areas and cost-increasing inefficiencies, the Statutory Health Insurance (SHI) Health Care Structures Reform Law was passed in 2012. This legislation has extended the opportunities of hospitals, to expand their outpatient services with medical care centers (§ 95 SGB V), outpatient treatment for regions with a shortage of medical services (§ 116a), ambulatory specialist care (§ 116b) as well as university outpatient departments (§ 117). In addition, § 115b of the Social Code Book V (SGB V) enables hospitals to offer outpatient surgeries. Both legislations allow hospitals to expand their range of services into the outpatient sector and to break away from the traditional sector structures. Therefore, the aim of the research project is to investigate, whether and to what extent German acute care hospitals are entering the ambulatory sector following the changes in legislation. In particular, the use of outpatient treatment possibilities by hospitals, concerning structural and contextual aspects, is analyzed.
The analysis is based on the following data sources: The structured quality reports of hospitals, the Diagnosis-Related Group Statistics of the Federal Statistical Office (DRG-Statistics) as well as data of the indicator-based spatial monitoring of the Federal Institute for Research on Building, Urban Affairs and Spatial Development (BBSR).
Scientific project leader
- Jun.-Prof. Dr. Lena Ansmann
- Prof. Dr. Holger Pfaff
Operative project leader
- Kira Hower
Cooperation partner
- Information and aid in drug issues e. V. Wesel, Jörg Kons and Sandra Groß
Funding institution
- Auridis GmbH
Duration
- 08/2015 – 12/2017
Project description
Currently, about 50,000 children of drug-addicted parents are living in Germany. Repeatedly the media reports tragic deaths of infants and young children of drug addicts. To consider the situation of children of addicts, an opening and widening of the activities of drug-counseling centers is necessary. So far, only 10% of the federal states have drug-counseling centers that offer activities directed to children of drug-addicted parents or that involve them in care planning. Accordingly, drug counseling is not prepared to care for children of addicts.
A few years ago, the drug-counseling center Wesel developed a program to embed the needs of children into the work of drug-counseling centers – the Fitkids program. This program provides a supportive framework and manual to continuously keep the conversation about children running and to create possibilities for training, information, and implementation support. The process evaluation of the pilot phase in 2011 and 2012, in which the program has been implemented in 7 locations, showed that the structured process of Fitkids is practical and realistic (more information can be found here: http://www.fitkids-wesel.de/).
In 2015, the program will be implemented in about 13 additional drug-counseling centers, considering important principles of organizational development and change management. The IMVR is now engaged to evaluate the effectiveness and the implementation of the program in the newly recruited locations.
The summative evaluation consists of two modules:
Quasi-experiment with pre-post design
The quality of the implementation and the effectiveness will be explored in a summative evaluation. Regarding the implementation, the following aspects are of interest:
- Implementation barriers and facilitators
- Principles of good implementation
- Readiness for change among employees
- Development of structures and processes for children orientation
- Workload and work climate
Regarding the quality of results, the following aspects are of interest:
- Children orientation
- Network orientation
- Satisfaction and acceptance of employees and parents
- Image of counseling centers
- Professional confidence
In a quasi-experimental study with pre-post design both the managers of the counseling centers and the employees will be surveyed before the start of the program (t0) and one year after program start (t1) using a standardized questionnaire. Survey data will be linked and compared between both time points.
Pilot sites as a reference group
In the second survey (t1), 16 other counseling centers are included. These so-called “pilot sites” are counseling centers that have been involved in the process evaluation of the pilot phase of Fitkids. These counselling centers implemented the Fitkids program longer than one year ago. The goal of taking the pilot sites into consideration is to examine the long-term implementation success as well as the implementation determinants. The results provide indications for the long-term success of Fitkids and give indications for the duration of its implementation.
Information and results
Key figures manual (german): EvaFit Kennzahlenhandbuch_EVA-TOM
Factsheets (german): EvaFit Studie, Evafit I, Evafit II
Hower, K.I., Pförtner, T.-K., Pfaff, H., Lee, S.-Y.D., Ansmann, L. (2019). Child-orientated drug counselling in Germany: Evaluating the implementation of the program “Fitkids” and its association with readiness for change. Human Service Organizations: Management, Leadership & Governance. DOI: 10.1080/23303131.2019.1661929
Bothe, P., Pfaff, H., Hower, K., Kons, J., Groß, S., Ansmann, L.: Organisationsentwicklung in der Sozialen Arbeit. Evaluation eines Programmes zur Förderung der Kindergesundheit in der Drogenberatung. Zeitschrift für Evaluation 2016; 15(1): 122-132.
Hower, K., Ansmann, L., Pfaff, H.: Die Veränderungsbereitschaft als Determinante des Implementierungserfolgs: Ein Projekt zur Evaluation eines Organisationsentwicklungsprogramms in der Drogenberatung. German Medical Science 2016: DocFV32, DOI: 10.3205/16dkvf027.
Project leader
- PD Dr. Mirjam Körner
- Dr. Christoph Kowalski
Project execution
- Jun.-Prof. Dr. Lena Ansmann
- Dr. Nadine Scholten
Collaboration partner
- Working group Health Services Research of the German Society of Medical Sociology (DGMS)
Duration
- 06/2014 – 07/2017
Project funding
- DFG gefördertes wissenschaftliches Netzwerk
Project description
The overall aim of health care delivery is to ensure that all patients receive effective, efficient, safe and humane health care. This requires the assessment of different levels of health care delivery like individuals, organizational units and organizations themselves.
In this research field of “organizational behavior” formal organizations, the behavior of persons in these organizations, the development of organizations as well as their purpose, context and environment are examined. The members of the network NWOB aim to capture the current state of research on organizational behavior in health care organizations in Germany and to sum them up with theoretical approaches, methods and empirical results. The network group comprises 15 researchers from various research fields and faculties of different universities in Germany (medical psychology, medical sociology, health care management, psychology, business administration, national economy, general medicine and health services research). Articles of all these researchers will be assembled to a systematic overview, published as an English-speaking book. Moreover, a review on the current state of research on organizational behavior in health care organizations in Germany will be conducted.
The intended result is to increase and establish the research on organizational behavior in health services research in Germany and thus to compete with international research in this field. NWOB aims as well to strengthen the collaboration between the researchers by building a research network for joint research proposals and projects.
Antragssteller
- Prof. Dr. Holger Pfaff
- Prof. Edmund A. M. Neugebauer, Private Universität Witten/Herdecke gGmbH (Department für Humanmedizin)
- Dr. Frank Vitinius, Uniklinik Köln (Klinik und Poliklinik für Psychosomatik und Psychotherapie)
- Prof.Dr. Stefan Wilm , Universitätsklinikum Düsseldorf (Institut für Allgemeinmedizin)
Project duration
- 2013 – 2016
Project funding
- Deutsche Forschungsgemeinschaft (DFG) – Projektnummer 244493120
Project description
The nature and quality of communication between primary care physicians and patients have a significant impact on the success of treatment. In many nations, including Germany, doctor-patient communication is still in need of improvement. The present research proposal aims to develop a communication training specifically tailored to family physicians. The theoretical basis of this training is the internationally established Four Habits Model, which is to be adapted to the conditions of German primary care. In order to adapt the communication training to the needs of patients and physicians in German primary care practices, focus group discussions will be conducted with both patients and primary care physicians to determine the specific requirements for communication training.
As a result, a customized communication training for German GPs will be designed. This training will be implemented, evaluated and further developed in a subsequent triple feedback process with small groups of GPs. Through a pretest in the GP practice, the feasibility of a video documentation and evaluation will be worked out, in which the developed training will be tested for its effectiveness. The goal of the project is to develop an effective communication training for family physicians. In a subsequent project (follow-up application), the communication training will be tested for its effectiveness in a randomized controlled trial.
Scientific direction
Project execution and contact person
Duration
- 03/2015 – 2016
Project funding
- The study is funded by the IMVR
Project description
Quality deficits such as interface problems, hygiene shortcomings or double diagnostics in service providers often root in problems related to the system of care provision rather than the involved individuals. Improving quality within the health and social care sector hence requires changes and transformations to the management, quality assessment and financing of the organization. Quality improvement should hereby avoid further investment (in terms of money or human resources) and rather focus on the reorganization of the system. The methods of lean management, firstly developed in the automotive industry, intend to reach the customer’s needs through efficient and slim organization of the work processes. For some time already, lean management is applied to the health care sector. Value Stream Mapping (VSM) is one of the methods of lean management. It can be used to visualize, quantify and thereby improve complex workflows. Service provision within the services sector differs from the industrial sector. In order to solve these challenges and to implement the method in care facilities a detailed understanding of Value Stream Mapping and its impact is essential.
Yet so far, there is no systematic review about the implementation and effectivity of Value Stream Mapping in care facilities. Some papers about the usage of VSM in the health care setting can be found, e.g. within emergency departments or multidisciplinary clinical operations. The present project aims to investigate whether Value Stream Mapping is an evidence-based method of organizational development which can be used in care facilities.
Publications
Nowak, M.; Pfaff, H.; Karbach, U.; Does Value Stream Mapping affect the structure, process, and outcome quality in care facilities? A systematic review. Systematic reviews Volume:6 Issue:1 Pages:170 2017; DOI: 10.1186/s13643-017-0563-y Link zum Volltext
Project management
Duration
- 11/2014 – 01/2016
Project funding
- The study is funded by the IMVR
Project description
In an ageing society, the burden of dealing with cancer and other chronic life threatening diseases increases. The aim of palliative care, as an interdisciplinary profession, is to provide symptom control and support for affected patients who are facing a terminal illness and their families. As quality of life, physical and psychosocial symptoms in cancer and non-cancer patients can be improved by palliative care, it is necessary to integrate it with other treatments early on. In the U.S., various organizations (e.g. the Institute of Medicine (IOM) and the American Society of Clinical Oncology) have promoted such integration. In Germany, where frequent public discussions about medical assisted suicide have been held, access to palliative care has also become an important issue. Although the demand is apparent, little is known about access to care in Germany. The aim of our study is to give a comprehensive picture of the regional inpatient palliative care situation in Germany, to examine what kind of hospitals provide palliative care and the disciplines into which palliative care is integrated.
Our study is based on the structured quality reports from 2012 which German hospitals are obliged to publish. The analysis on the patient-level, regarding length of stay or main and secondary diagnosis, are being performed with data from the federal bureau of statistics (DRG statistics 2012).
Project direction
- Univ.-Prof. Dr. Stephanie Stock (Institute for Health Economics and Clinical Epidemiology (IGKE) at the University of Cologne)
- Jun.Prof. Priv.-Doz. Dr. Nicole Ernstmann
Project execution
- Sibel Altin (Institute for Health Economics and Clinical Epidemiology (IGKE) at the University of Cologne)
- Sarah Halbach
Cooperation partner
- Univ.-Prof. Dr. Christian Rietz (Department of research methods at the University of Cologne)
Duration
- 01/2014 – 12/2015
Funding institution
- UoC-Forum Universität zu Köln
Project description
International studies show that inadequate health literacy is associated with increased mortality and morbidity rates, higher rates of hospitalizations as well as an avoidable use of health care services and therefore avoidable costs. In order to improve health literacy, strategies and instruments are required that are adapted to the needs of the respective targeted population. In Germany, there is a lack of sub-group analyses that are focused on the determinants and effects of inadequate health literacy in the chronically ill. Furthermore there are no instruments that measure health literacy and cancer literacy in the context of the German health care system.
In this project that is conducted in cooperation between the IGKE and the IMVR the following aims are pursued. First, determinants of inadequate health literacy of breast cancer patients in Germany are to be identified. Therefore explorative analyses are conducted to investigate the association between socio-demographic, personal and health-related characteristics and inadequate health literacy in the breast cancer patients. Second, the economic consequences of low health literacy on health care utilization and costs are analysed. Third, the constructs of health literacy and cancer literacy are to be defined from the cancer patients’ perspectives. Based on these results it is planned to develop an instrument to measure these constructs. Fourth the association between health literacy and fear of progression is investigated.
The analyses are based on quantitative data of the breast cancer patients from the PIAT-study, data from the health insurances as well as qualitative data that is generated in focus groups with patients recruited from the PIAT-study.
Results
Altin, S.V., Halbach, S., Ernstmann, N., Stock, S. (2015). Wie können krebsspezifische Gesundheitskompetenzen gemessen werden? – Ein systematischer Review über die Qualität vorhandener Messinstrumente. Z. Evid. Fortbild. Qual. Gesundh. wesen (ZEFQ).
Project director
- Prof. Dr. Holger Pfaff
- Dr. Frank Verheyen, Director of WINEG – TK Scientific Institute of TK for Benefit and Efficiency in Health Car
Project execution
- Anna Enders
- Dr. Nadine Scholten
- Brigitte Grenz-Farenholtz
- David Zach
Duration
- Start in January 2010, estimated completion in late 2015
Funding institution
- WINEG – Wissenschaftliches Institut der TK für Nutzen und Effizienz im Gesundheitswesen
Project description
The scientific study on the state of health services research in Germany is designed to increase the transparency regarding research results and competencies in the area of preventive and curative healthcare. The systematic Germany-wide registration of projects in health services research within a project database offers a platform that health services researchers can use to exchange information and gain insights. The research results and the identification of best practice models provide a scientific basis for decision-making regarding patient care structures and serve to improve and more rapidly implement new care models into daily practice. In addition, practical implementation is facilitated by enabling stakeholders to more easily locate the findings from health services research. Numerous high-quality projects relevant to health services research are documented in the database. These projects can contribute to the transfer of knowledge and stimulate the discussion of health services research results
Projectgroup Wirtschafts- und Sozialwissenschaftliche Fakultät
- Prof. Dr. Ludwig Kuntz (Seminar für ABWL und Management im Gesundheitswesen)
- Dr. Michael Wittland (Seminar für ABWL und Management im Gesundheitswesen)
- Hendrik Hillen (Seminar für ABWL und Management im Gesundheitswesen)
- Dr. Hendrik Wilhelm (Seminar für ABWL, Unternehmensentwicklung und Organisation)
Projectgroup Medizinische Fakultät
- Dr. Nadine Scholten
- Prof Dr. Bernard Roth (Klinik und Poliklinik für Kinder- und Jugendmedizin, Bereich Neonatologie)
- PD Dr. Angela Kribs (Klinik und Poliklinik für Kinder- und Jugendmedizin, Bereich Neonatologie)
- Kyriakos Martakis (Klinik und Poliklinik für Kinder- und Jugendmedizin, Bereich Neonatologie)
Duration
- 2015
Project Funding
- UoC-Forum Universität zu Köln
Project description
Aside from structural parameters (e.g., staffing), the quality of medical care is influenced by many other determinants. Concerning the intensive care of newborns, teamwork between inter-professional teams is especially important. Besides effective cooperation between and within the professions, the safety climate seems to be a relevant determinant influencing the quality of care. Mostly, in an NICU in Germany, there is a collective leadership between the head nurse and the medical leader of the department (leadership-dyad). In the literature, it has been shown that leadership skills have a significant influence on team performance. What has not been sufficiently analyzed before is the role of leadership skills in leadership-dyads. Here, concordant personal goals and affection during interactions can have an influence on the subordinated team. Therefore, the aim of our study is to explore the relationship between leadership skills of the managers on the safety and team climate within the NICU. Besides leadership skills, our model includes the concordance of selected goals between the leadership-dyad and the interpersonal effects occurring with interactions. The AQUA quality indicators, which are collected for external quality assurance, are used to measure the department’s quality of care.
The project is planned as a two-stage, prospective, questionnaire-based multi-center study. Two different questionnaires will be developed: one for the leadership team and one for the doctors and nurses working in the participating NICUs. All Level I and Level II neonatology centers in Germany will be included in the study. As of July 2014, there are 243 neonatology centers.
The sub-project, “Exploring Leadership Skills and Leader Team Configuration as Antecedents of Safety Climate and Climate for Collaboration, and their Effects on Neonatal Outcomes”, is part of the UoC Forum “Managerial Risk Factors in Medicine”, which is funded by the University of Cologne (Excellence Initiative).
More information about the UoC Forum and its sub-project, “Managerial Risk Factors in Medicine”, can be found here.
Project leader
- Prof. Dr. Ludwig Kuntz (Projektkoordinator), Universität zu Köln, Seminar für ABWL und Management im Gesundheitswesen
- Prof. Dr. Bernhard Roth, Uniklinik Köln, Abteilung Neonatologie
- Prof. Dr. Christiane Woopen, Uniklinik Köln, Forschungsstelle Ethik
- Prof. Dr. med. Dipl.-Kfm. (FH) Rainer Riedel, Rheinische Fachhochschule Köln, Institut für Medizin-Ökonomie und Medizinische Versorgungsforschung (iMöV)
- Prof. Dr. Holger Pfaff
- Dr. Annika Nitzsche
Project duration
- 02/2015 – 12/2015
Project funding
- Die Studie wird aus Eigenmitteln des IMVR finanziert.
Project description
Health care research on the treatment and care of preterm infants with a birth weight below 1500g – Influence of human and organizational factors on the performance of neonatal intensive care units.
Prematurity is the leading cause of perinatally acquired disability and mortality. The needs-based care of preterm infants with a birth weight below 1500g is shaped by various factors. The Health Services Research in Neonatal Intensive Care Units (HRS-NICU) research project, funded by the German Federal Ministry of Education and Research (BMBF) since 2012, addresses the question to what extent human and organizational factors have an impact on the performance of neonatal intensive care units.
In a pilot study at 5 German perinatal centers, workload, staff attitudes, and structural characteristics were found to be relevant variables influencing the outcome of preterm infants.
In the current interdisciplinary multicenter study, the relationships between medical outcome, working conditions, staff and parent satisfaction, economic outcome factors, goals and organizational processes are investigated in collaboration with medicine, ethics, business administration and sociology at 60 neonatal centers. Data collection will be conducted using staff and parent questionnaires, medical data, and general information (capacities, structures, shift schedules, costs).
The results expected from this interdisciplinary innovative project are expected to make a significant contribution to the health policy design of care structures and processes for the field of neonatology.
Project director
- Prof. Dr. med. Hans W. Höpp, HNC HerzNetzCenter GmbH
- Prof. Dr. Holger Pfaff
Project manager (German part of the project)
- Jun.-Prof. Dr. Nicole Ernstmann
- Dr. Ute Karbach
Co-operative partner
- Alere GmbH
- AOK Rheinland-Hamburg
- BARMER GEK
- IMO Institut GmbH
- Uniklinik Köln
Duration
- 09/2012 – 08/2015
Project funding
- Europäische Union und Ministerium für Gesundheit, Emanzipation, Pflege und Alter des Landes NRW im Rahmen des NRW-EU -Ziel 2 (EFRE) Förderwettbewerbs.
Project description
Structured health care programs generally result in greater adherence to guidelines during care, improved prognoses, better insight into illness and improved quality of life. However, access to relevant programs is often restricted by their very approach and structure. In addition, sociodemographic and psychological factors seem to be the most likely reason for the observation that nearly half of all medically suitable patient candidates for a particular program decide not to participate.
The aim of the GemaB project is, therefore, to study the influence of sociodemographic factors—particularly gender and ethnic origin—on the willingness of patients to participate in health care programs by examining an existing health care model for people with chronic heart failure. The task of the IMVR is to develop two questionnaires: 1) a questionnaire for assessing patient acceptance of the model, which will be used in structured telephone interviews to survey all male and female patients who are candidates for participation in the model based on their illness, and 2) a patient satisfaction questionnaire, which will be used to evaluate the model 12 months after patients have participated in it.
Project managers of the PIAT Study
- Jun.-Prof. Dr. Nicole Ernstmann
- Dr. Christoph Kowalski
Operational project manager
- Dr. Anna Enders (geb. Schmidt)
Student research assistant
- Isabell Schellartz
- Lara Schlomann
Collaborative partners
Duration
- 03/2012 – 03/2015
Funding institution
- Federal Ministry of Health (BMG) within the framework of the departmental research “Research in the National Cancer Plan”.
Project description
The aim of the PIAT Study is to analyze breast cancer patients’ needs for information and training measures which increase patient competence. In order to assess these needs, the prospective cohort study will involve a written survey of breast cancer center patients and directors conducted in three waves. The data collection instrument used for the survey will be developed based on a review of the literature and on focus groups conducted with patients and health care providing institutions. The main goal of the PIAT study is to assess the needs of breast cancer patients. The secondary goal is to analyze and establish links between the results from the various breast centers with respect to the study’s primary outcome variables. The study’s results will facilitate the development of information and training measures that are tailored to the needs of breast cancer patients and that take into consideration certain barriers and facilitating factors at the health care institution level.
Project director
- Prof. Hans Wilhelm Höpp
Project partner
Project execution
- Dr. Antje Hammer
Duration
- 06/2013 – 12/2014
Funding institution
- Foundation funds (iEVF)
Project description
The aim of the Köln (Cologne) Infarction Model is to examine the feasibility of obligatory treatment of ST-segment-elevation myocardial infarction (STEMI) by first-line percutaneous coronary intervention. All over the country it is a unique attempt to set up transsectoral standards in a megapolis with a complicated care structure.
The main purpose of the work package executed by the IMVR is the analysis of two research question: (1) To what extent time (time of day, season etc.) affects guideline-compliance in the treatment of KIM-patients? (2) Do KIM-patients with different socioeconomic backgrounds receive different treatment? To answer the questions we will analyse patient’s data collected since 2006 to present.
The project is funded by a charity (iEVF) and contains – in cooperation with Prof. Höpp – the supervision of two doctoral students.
Project leader
- Prof. Dr. Holger Pfaff
- Prof. Dr. Markus Wirtz (Institute of Psychology, Freiburg University of Education)
Project execution
- Lena Ansmann
Duration
- 11/2012 – 10/2014
Funding institution
- German Cancer Aid
Project description
Having a diagnosis of breast cancer and experiencing the associated side effects and burdens of treatment present breast cancer patients with various challenges. Supportive resources are needed in order to successfully face these challenges. A significant source of social support for breast cancer patients is a trusting relationship between physician and patient. Existing research on the significance of physician-patient communication with respect to chronic illnesses supports the association between the physician-patient relationship and patient-reported outcomes.
The WORG OUT research project investigates the influence of the health care setting on the communication between physicians and breast cancer patients by examining the extent to which patients’ perceived psychosocial care by physicians is related to hospital structures and processes. So far, little research exists on the influence of the hospital context on physician-patient interaction. Each year, the IMVR conducts surveys of patients treated in breast centers in the German state of North Rhine-Westphalia (NRW). The results of these surveys show that patients are very highly satisfied with most areas of care. There are, however, significant noticeable differences in patient assessments between the breast centers which cannot be attributed to patient differences alone. The WORG OUT project will attempt to explain the differences between these health care institutions, especially with regard to assessments of physician-patient interaction.
To investigate the research question, the project will use the method of organizational diagnosis and will apply multiple perspectives to analyze organizational issues. For the first time, data from surveys examining the NRW breast centers from different perspectives will be combined, namely survey data from an annual 3,000 – 4,000 female breast cancer patients, data from key person surveys conducted in 2007 and 2010, and data from a 2010 survey of breast center employees. The data will be analyzed through multilevel analysis.
The project’s findings will be used to formulate recommendations for improving physician-patient interaction at the organizational level of the breast centers. Dissemination of the findings will be ensured by providing the breast centers with feedback during a knowledge transfer workshop.
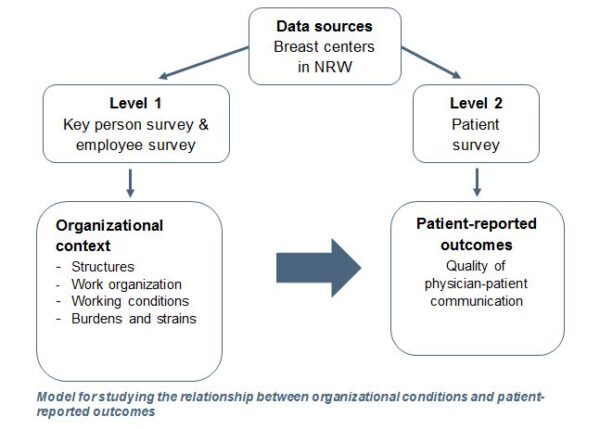
Scientific project leader of the WIN ON Study
- Jun.-Prof. Dr. Nicole Ernstmann
- Dr. Melanie Neumann (UniversityWitten/Herdecke)
- Prof. Dr. Holger Pfaff
- Prof. Dr. Markus Wirtz
Scientific project leader at the IMVR
- Jun.-Prof. Dr. Nicole Ernstmann
Project collaborators at the IMVR
- Anika Nitzsche (Operation project leader)
- Lena Ansmann
- Tristan Gloede
- Sophie Groß
Co-operative partner
Duration
- 03/2011 – 12/2013
Funding institution
- Deutsche Forschungsgemeinschaft (DFG) und Köln Fortune
Project description
The WIN ON (Working Conditions in Oncology) research project is concerned with determining the impact of organizational structures and processes in the practices of private-practice hematologists and oncologists (PPOs) on the way these physicians experience their work, on their communication with patients and on patient-reported outcomes (e.g., quality of life).
In a qualitative pre-study, PPOs were interviewed about their working conditions, their health, their communication with patients, and their self-assessed communication skills. Standardized questionnaires on the above-mentioned topics were then developed based on the results of the qualitative pre-study. The questionnaires were used in a nationwide survey of PPOs. Patients with colorectal cancer being treated by these physicians are also surveyed as part of a four-wave prospective study. In the patient surveys data on patients’ expectations of their physicians and consultations, on their perceptions of the communication with their physicians and on patient-reported outcomes are collected over a period of six months.
Publications
Groß, S.E., Ernstmann, N., Jung, J., Karbach, U., Ansmann, L., Gloede, T.D., Pfaff, H., Wirtz, M., Baumann, W., Schmitz, S., Osburg, S., Neumann, M. Can a stressed oncologist be good in a consultation? A qualitative study on the oncologists’ perception. European Journal of Cancer Care DOI: 10.1111/ecc.12199
Ansmann, L., Nitzsche, A., Neumann, M. Gestresst, aber zumeist zufrieden (2014). Deutsches Ärzteblatt, 111(7):A262-264.
Project director
Project execution
- Anika Nitzsche
Partner
- Prospektiv GmbH
- IVAM e.V.
Model companies
- Bartels Mikrotechnik GmbH
- LIMO Lissotschenko Mikrooptik GmbH
- NanoFocus AG
Duration
- 07/2009 – 04/2013
Funding institution
- Federal Ministry of Education and Research
- European Social Fund for Germany
- European Union within the framework of the program “Working, Learning, Developing Competencies – Innovative Capability in a Modern Working World”
Project description
Background: The German microtechnology and nanotechnology industries represent a fairly young and dynamic growth sector that acts as a driver of innovation and of considerable industrial added value. The need for skilled employees is growing in the microtechnology and nanotechnology industries, and the field is characterized by professions with highly specific knowledge that is critical to success. These professions regularly experience rapid changes. Therefore, continual participation in (additional) training is absolutely necessary. In addition, the highly intense competition in a globalized market with ever shorter product cycles and the diffusion of new technologies as well as the social and demographic developments in society put companies in this sector under great pressure to change: Flexibilization is the major challenge. This situation results in a relatively high level of demands and stress for these highly qualified employees. In addition, the retention of existing employees and the recruitment of new professionals is an existential challenge for companies.
Goals: The overall goal of the collaborative “GeMiNa” project is to create a balance between flexibility and stability through implicit agreements in the microtechnology and nanotechnology industries. For this purpose, concepts regarding work-life balance are created, implemented, and later evaluated in model companies using the psychological contract as a tool.
Work-Life-Balance: In the future, microtechnology and nanotechnology companies will only be successful if they invest in their most important resource – their employees. Performance and success factors include qualifications and knowledge, but also an intact balance between work and private life, referred to as work-life balance (WLB). Employees and companies equally benefit from a good WLB. Companies can benefit in terms of gaining a competitive advantage, for instance, by increasing their attractiveness as employers, which helps them to recruit and retain professionals. Furthermore, WLB-promoting measures can contribute to increased employee commitment, motivation, and satisfaction. In addition, effects on physical and psychological health indicators (e.g., physical complaints, depression, and burnout) have already been demonstrated, so that supporting a good WLB can make an important contribution to the promotion of employee health, which ultimately also reduces absences.
The psychological contract as a tool to improve work-life balance: Although it is already a popular concept in Anglo-Saxon countries, the psychological contract is not yet in common use in Germany. Psychological contracts include numerous mutual expectations between employees and employers that are not specified in the formal employment agreement. Until the late 1990s, psychological contracts included typical topics such as job security, opportunities for promotion, etc., on the employee side, and quality work, loyalty, flexibility, commitment, etc., on the employer side. But as a result of progressive flexibilization measures taken by the companies and rising market demands, psychological contracts have changed as well. For example, personal responsibility for employment has replaced job security. Employees taking responsibility for their own marketability and professional development replaces company-specific specialization and internal promotion opportunities. The “classic” psychological contract no longer applies. As a consequence, employees feel less of a personal connection to the company and become less dedicated. Scientific studies demonstrate this systematic transformation of the implicit agreement “job safety in return for high commitment and flexibility.” Companies are replacing job security with continuous promotion of employability. This requires that employees take significantly greater responsibility for their own development (“entreployees”).
Approach:
- Qualitative preparation: Guided interviews with employees and managers in the microtechnology and nanotechnology industries
- Analysis of current conditions in three model companies as well as in other companies within the industry: Online inventory designed to take an inventory of the framework conditions as well as the mutual offerings and expectations in aspects related to work-life balance, workload, etc., using an online survey
- Conduction of workshops on work-life balance and the implementation of measures in three model companies
- Evaluation: Analysis of the effectiveness of the psychological contract as a tool for improving work-life balance using another survey (panel design)
Konwledge Transfer: The outlined project is developed and implemented in collaboration with three model companies in the microtechnology and nanotechnology industries. In a first step, the model companies are encouraged to exchange experiences. This exchange is later expanded to interested companies within the industry (value partners). In the context of the transfer, interim and final results are professionally prepared for presentation in a manner tailored to the industry. For this purpose, a project website, additional informational materials, and a practical guide are created. The guide is intended to include many important notes and insights on how to design and implement psychological contracts. In collaboration with the IVAM Microtechnology Network as well as other partners, these results are made widely available. The results are intended to benefit the “original industries” of microtechnology and nanotechnology but also to be transferred to other, related industries who are also characterized by a high proportion of “knowledge workers” (IT, media, etc.). .
Project execution
- Jun.Prof. Dr. Nicole Ernstmann
Duration
- 03/2011 – 07/2013
Project funding
- The study is funded with IMVR’s own resources
Project description
There is an increasing body of knowledge to the needs and preferences of prostate cancer patients, however, little is known to the changes in communication and the relationship between provider and patient over time. The present study, using a qualitative approach, was designed to improve our knowledge and understanding of changes over time in the provider-patient-interaction during prostate cancer treatment. Since prostate cancer treatment and follow up-care often lasts over years it is the aim of our study to understand in depth changes of patients’ communicative and supportive care needs and changes in the relationship between provider and patient over time. In order to recruit patients in different stages of the disease and with experiences of different treatment options in different settings patients will be recruited in a support group in the area of Cologne. Semi-structured interviews following an interview guideline will be conducted with 12-15 patients.
Project leader
Duration
- 12/2011 – 12/2013
Project funding
- The study is funded with IMVR’s own resources
Project description
According to the guidelines acute stroke patients should be treated in hospitals specialized in the treatment of stroke patients. The purpose of this study is to describe and cartographically analyze the medical treatment situation of stroke patients in Germany by using routine data. Possible disparities between urban and rural regions, concerning the thrombolysis rate are being statistically evaluated.
Data sources are the structured quality reports of the years 2008 and 2010, which according to §108 SGB V, have to be published by all hospitals performing medical treatment. For the year 2010 we were able to include the data of 1300 different hospitals (194.000 stroke patients with the diagnosis I63 ICD-10-GM) into our statistical analysis. By performing logistic regression (STATA 12) possible correlations between hospital characteristic (e.g. hospital location, number of beds, number of stroke patients) and the performance of thrombolytic therapies are being detected. Possible regional deficits in the treatment of stroke patients are being identified by performing cartographic methods.
Project director (German part of the project)
- Prof. Dr. Holger Pfaff
- Dr. Oliver Ommen, MPH (deputy)
Project manager (German part of the project)
- Antje Hammer
Contact (German part of the project)
- Antje Hammer
Duration
- 11/2009 – 04/2013 (extended until 08/2013)
Project funding
- DUQuE is funded by the EU DG Research Grant in the 7th Framework Programme. In addition, the German part of the project is financially supported by Köln Fortune.
Project description (overall project)
The project’s objective is to examine the effectiveness of quality improvement measures in European hospitals. For this purpose, the project studies the relationships between quality improvement measures, institutional culture, involvement of occupational groups, and patient empowerment on one hand, and the quality of hospital care (including clinical effectiveness, patient safety, and patient involvement) on the other.
A total of 240 European hospitals in 8 countries (Germany, France, Poland, Portugal, Spain, Turkey, Czech Republic, and the United Kingdom) will participate in the study. A random sample of 30 hospitals in each country will be selected for data gathering. In the randomly selected hospitals, surveys are distributed to various professional groups (e.g., physicians, nurses, managers). The survey is conducted using uniform questionnaires for each professional group. They will include hospital-specific questions for the assessment of parameters affecting hospitals, such as external demands, hospital management, quality improvement measures, patient empowerment, institutional culture, and involvement of professional groups.
In 12 these 30 randomly selected hospitals, additional data are collected on the patient level, e.g., on patient safety and patient involvement. Further, 12 hospitals are planned to undergo external audits.
The results of this project are used to develop guidelines for hospital management as well as for purchasing cooperatives and authorities that are involved in the development and assessment of systems for the improvement of hospital quality in Europe. On the basis of the research results, practice-based tools are developed that serve to further optimize quality improvement systems in hospitals. Further, additional quality criteria are developed for the future awarding of contracts in the context of the supply of hospital care.
Coordination and partners
Avedis Donabedian University Institute, Autonomous University of Barcelona.
Project coordination: Rosa Suñol. Oliver Groene (assistant): Avedis Donabedian University Institute, Autonomous University of Barcelona.
Partners: Academic Medical Centre (AMC) (Niek Klazinga); Netherlands Institute of Health Services Research (NIVEL) (Cordula Wagner); Dr Foster Intelligence (DFI) (Tim Baker); Central Denmark Region (RM) (Paul Bartels); University of California in Los Angeles (UCLA) (Onyebuchi Arah); Institute of Medical Sociology, Health Services Research and Rehabilitation Science (IMVR) (Holger Pfaff); European Hospital and Healthcare Federation (HOPE) (Pascal Garel); European Society for Quality in Healthcare (ESQH) (Basia Kutryba).
Country coordinators: Czech National Accreditation Committee (František Vlček); Haute Autorite de Santé (Charles Bruneau); Polish Society for Quality Promotion in Health Care (Halina Kutaj-Wasikowska); General Directorate of Health (Margarida Franca); Foundation for the accreditation and the development of health services (Paula Vallejo); Turkish Society for Quality Management (Hasan Kus); Dr Foster Intelligence (Ellen Klaus / Alex Kafetz)
Additional information
Scientific director of the HAROW study
- Prof. Dr. Lothar Weißbach, Stiftung Männergesundheit
Scientific director of the ZVFK subproject
Executing research offices
- Clinische Studien Gesellschaft mbH (CSG) mediq.us GmbH
- Cologne Center for Health Services Research (ZVFK)
Operational project management of the ZVFK subproject
- Jun.-Prof. Dr. Nicole Ernstmann
Duration
- 03/2008 – 03/2013
Project description
Prostate cancer represents 20% of all new cancer cases in men. Although these tumors grow slowly, prostate cancer is responsible for about 10% of all cancer deaths in men. In Germany, about 11,000 men die of this type of cancer every year. The treatment of prostate cancer depends on the spread of the tumor, its stage or degree of malignancy, and the patient’s age and health status. The treatment type should be selected together with the patient after he has been comprehensively informed about the risks and benefits of the individual treatment options. A personal conversation between the physician and the patient is the preferred method of conveying this information. Studies show that the compliance and adherence of patients with localized prostate cancer depend on the selected treatment type. There is evidence that prostate cancer patients favor less invasive procedures, which are associated with a comparatively minor reduction of the health-related quality of life. When prostate cancer is diagnosed, it is therefore particularly important to identify the specific relationship between prostate cancer’s natural course of disease and the patient’s personal life expectancy. Five major treatment strategies are differentiated for the stage of localized prostate cancer; they have not yet been clearly classified in terms of superiority: H = Hormones, A = Active Surveillance, R = Radiotherapy, O = Operation and W = Watchful Waiting.
The HAROW study therefore aims to describe the current health services situation in Germany and to prospectively examine the course of disease associated with each treatment strategy. For this purpose, the HAROW study is designed as an open, non-interventional observation study. We plan to include 5,000 patients with newly diagnosed, localized prostate cancer.
In the context of the HAROW study, the ZVFK is responsible for the measurement and analysis of relevant aspects of the physician-patient interaction from the patients’ point of view. Treatment satisfaction, trust in the urologist, and physician empathy, and the quality of psychosocial care will be examined.
Project leader
- Prof. Dr. Holger Pfaff
- Akademischer Oberrat Dr. med. Oliver Ommen, MPH
Duration
- 02/2008 – 03/2012
Project funding
- Deutsche Forschungsgemeinschaft (DFG)
Project description
On the basis of the previous studies on psychotherapeutic intervention in trauma victims, the project aims to develop, practically test, and evaluate a comprehensive concept for the psychosocial care of trauma victims. The intervention program Advanced Trauma Psychosocial Support (ATPS) was modeled after Advanced Trauma Life Support (ATLS) created by the American College of Surgeons, and it establishes a standardized procedure for the psychosocial care of trauma victims. ATPS consists of two parts: The first part is a training concept for physicians working in the field of trauma surgery that includes a general module on basic skills for physician-patient communication and a module on the specific psychosocial situation of trauma surgery patients. The latter provides the physician with the expertise to properly respond to psychosocial problems and to identify patients with psychopathological reactions while they are still at the hospital.
The second pillar of Advanced Trauma Psychosocial Support (ATPS) consists of offering these identified patients a psychotherapeutic intervention that is specifically tailored to the symptoms and needs of trauma patients. In the context of the study, the effectiveness of ATPS will be evaluated using a pre-post design over a period of 36 months. The study measures whether the training improves the communication behavior of trauma surgeons on a sustained basis, how the improved communication behavior affects the psychosocial care of the patient (trust in physicians), and whether the physicians have gained psychosocial diagnostic expertise for identifying symptomatic patients. Furthermore, the effects of psychotherapeutic intervention are analyzed, and its suitability for the treatment of the specific symptoms of trauma victims is evaluated.
ATPS is a cooperative research project with the Institute for Research in Operative Medicine (IFOM) of the University of Witten / Herdecke (project manager of the IFOM study part: Prof. Dr. Rolf Lefering.)
Project director
Project execution
- Christoph Kowalski
- Lena Ansmann
Duration
- 04/2010 – 03/2012
Project description
In the context of the introduction of the breast center concept in North Rhine-Westphalia, the Ministry for Labor, Health and Social Affairs of North Rhine-Westphalia (MAGS-NRW) funded a study conducted from July 2006 to December 2008 with the goal of documenting the changes in the structures and processes of breast cancer care in NRW and studying their effects on treatment outcomes. The study was conducted by scientists of the University of Cologne Medical Center, the Ruhr-Universität Bochum, and the University of Düsseldorf with support from the Westfalen-Lippe Medical Association.
The final report gave rise to further questions that could not be fully answered with the available data. A follow-up project named EBRU II was initiated to provide additional information on the implementation of requirements, on the staff’s perspective, and on potential relationships with the quality of care as perceived by patients. This project included both a follow-up survey of key persons in the breast centers and a survey of the staff responsible for patient care. EBRU II is funded by the Healthcare Campus North Rhine-Westphalia – Healthcare Strategy Centre. The additional survey performed at the breast centers is intended to examine medium-term changes and their impacts and determine to what degree the implementation of certain requirements sustainably affects the quality of care as perceived by patients. The data can be directly linked to those of the initial survey. The staff survey is intended to examine the effects of the introduction of the new concept on the organizational workflows and the organizational climate. The two modules designed to examine the medium-term impact of the introduction of the breast center concept on the quality of care and on the organization and climate of the facilities include the following:
1.st module: Follow-up survey of key persons at the breast centers (follow-up survey of hospital administration): Two-and-a-half years after the initial survey, the implementation status of the criteria catalog has been examined again using a largely identical questionnaire. The survey has been conducted in the summer of 2010.
2.nd module: Survey of the surgery facility staff who care for patients with primary breast cancer: The staff members have been surveyed using established and uniform indicators, some from the Cologne employee indicators form (MIKE) (Pfaff et al. 2004), others from German and international research, and still others developed specifically for this survey. The survey has been conducted between November 2010 and March 2011.
Project director
Project execution
- Anika Nitzsche
- Julia Jung
- Birgit Lehner
Duration
- 10/2007 – 10/2010
Project description
“PräKoNeT,” a three-year joint-project commissioned by the BMBF, is conducted under the combined leadership of Core Business Development GmbH, the University of Cologne (Department of Medical Sociology as well as the University of Duisburg-Essen (Department of Medicine Management) and collaboration of many partners such as companies, health insurances, expert committees, and other working groups. One of the focuses of the project is the preservation of the innovative employability of skilled ITC personnel for the duration of their professional life by integrating health promotion that is relevant to knowledge work.
The overall goal of the joint project is to develop, implement, and promote a new dimension of preventative occupational safety and health through a sustainable alliance of actors in order to then integrate this new dimension into the innovation strategies of ITC companies. The following subgoals will be pursued over the course of the project:
- Assessment of the prevention capacity in more than 500 ITC companies.
- Participative development of innovative design solutions for workplace health promotion programs through personnel and expertise development as well as through organizational restructuring and corrective job designs of the knowledge-based work activities in ITC companies, according to their level of prevention capacity.
- Implementation and design of the developed concepts for workplace health promotion in ITC model companies based on the determined prevention capacity by using innovative instruments for knowledge communication.
- Implementation of selected solution strategies to overcome typical stress situations arising in ITC knowledge work (e.g., option stress) in ITC companies with a high prevention capacity by providing these companies with experiential knowledge. Economic evaluation of the cost-benefit ratio necessary.
- Qualitative assessment and economic evaluation of the implemented solution strategies. Cost-effectiveness evaluation using a (simulation) model. Test the potential transferability of the model to focus group projects over the course of the main PräKoNeT project.
- Goal-oriented broad knowledge transfer of the developed findings and experiences gained both between the ITC companies, by way of the work groups and expert committees
Further information can be found on http://www.praekonet.de

